What Causes It?
Genetic predisposition: Specific HLA-DQ2 and HLA-DQ8 genes increase susceptibility
Environmental triggers, with gluten being the primary trigger
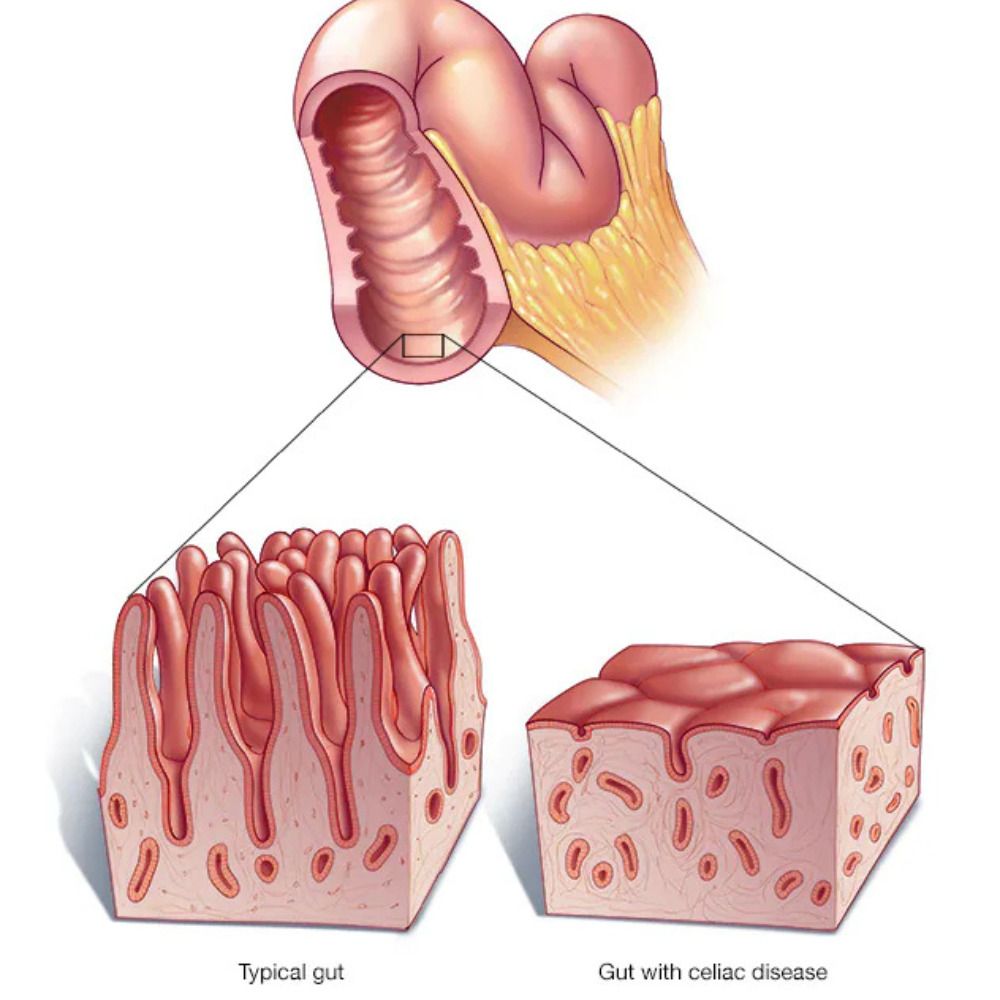
Autoimmune reaction where the body's immune system mistakenly attacks its own tissues
Family history (first-degree relatives have a 10-15% higher risk)
Other autoimmune disorders (type 1 diabetes, autoimmune thyroid disease, etc.) increase risk
Viral infections or gut bacteria changes may contribute to onset in genetically predisposed individuals
Timing of gluten introduction in infancy (controversial)
Pregnancy can sometimes trigger or unmask celiac disease
Emotional stress or trauma may trigger onset in susceptible individuals
Surgery, particularly gastrointestinal surgery
Signs & Symptoms
Digestive symptoms: diarrhea, bloating, gas, abdominal pain, and nausea
Weight loss or difficulty gaining weight despite adequate food intake
Malnutrition leading to anemia (iron, folate, or B12 deficiency)
Fatigue and weakness
Bone or joint pain
Arthritis
Osteoporosis or osteopenia due to calcium and vitamin D malabsorption
Dermatitis herpetiformis (itchy, blistering skin rash)
Headaches or migraines
Neurological problems including ataxia, seizures, or peripheral neuropathy
Reproductive issues: infertility, recurrent miscarriages, or late onset of menstruation
Dental enamel defects
Depression, anxiety, or "brain fog"
Growth problems or delayed puberty in children