What Causes It?
Weakened lower esophageal sphincter (LES), which normally prevents stomach contents from flowing back
Hiatal hernia, where the upper part of the stomach bulges through the diaphragm
Obesity or being overweight, which increases pressure on the abdomen
Pregnancy, which temporarily increases pressure on the abdomen
Smoking, which can impair LES function and increase acid production
Regular use of certain medications, including aspirin, ibuprofen, and some muscle relaxants
Consuming large meals or lying down right after eating
Dietary triggers such as spicy foods, fatty foods, citrus, chocolate, mint, and carbonated beverages
Alcohol consumption
Delayed stomach emptying (gastroparesis)
Signs & Symptoms
Heartburn - a burning sensation in the chest, typically after eating
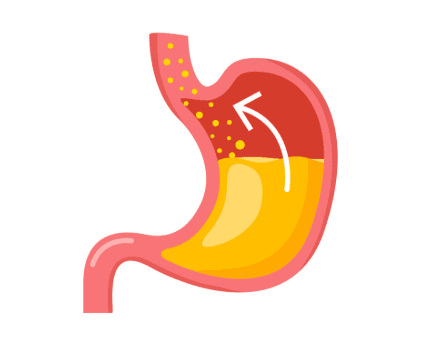
Regurgitation of food or sour liquid into the throat or mouth
Chest pain, particularly when lying down
Difficulty swallowing (dysphagia)
Sensation of a lump in the throat
Chronic cough, particularly at night
Laryngitis or hoarseness, especially in the morning
Disrupted sleep due to discomfort
Worsening of asthma symptoms
Dental erosion from stomach acid exposure
Bad breath