What Causes It?
Hiatal hernia: Weakening of the diaphragm muscle due to age, injury, or congenital factors
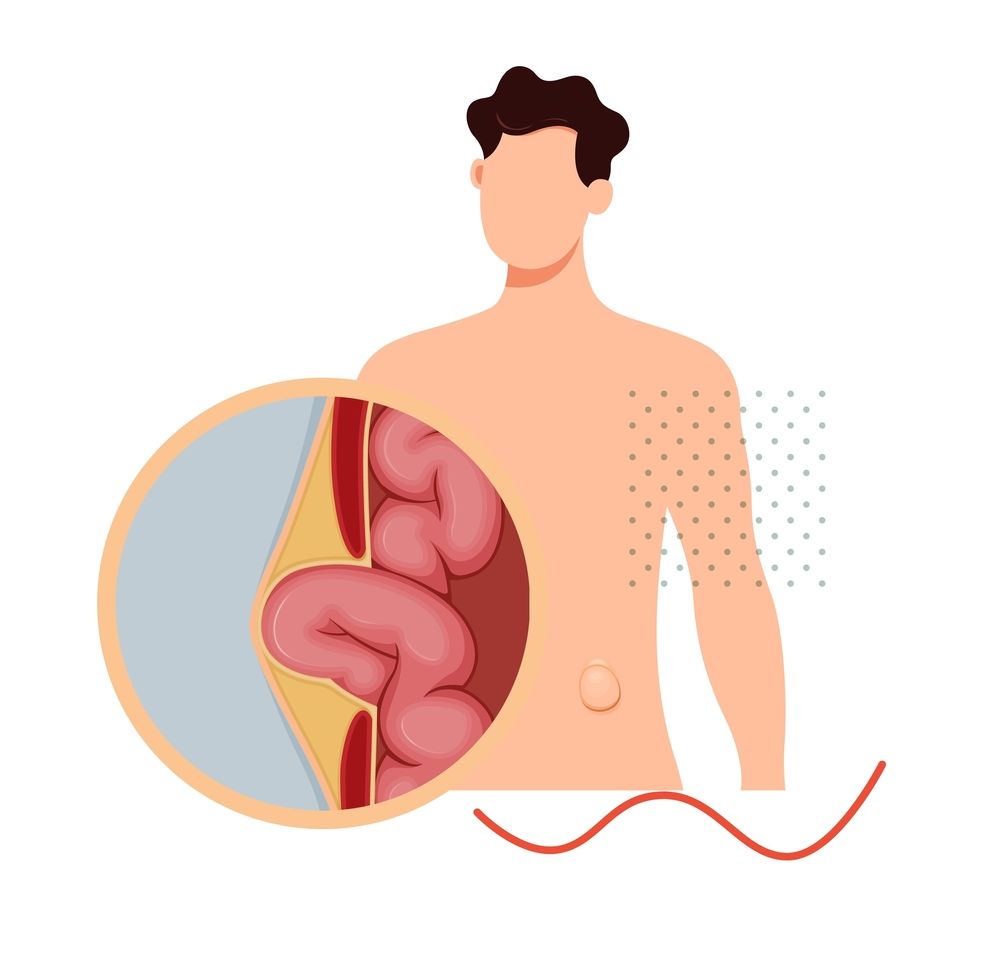
Inguinal hernia: Weakness in the lower abdominal wall, often at birth (congenital) or developing later in life
Umbilical hernia: Incomplete closure of the abdominal wall at the umbilicus during development
Incisional hernia: Weakness at the site of previous abdominal surgery
Increased abdominal pressure from chronic coughing, straining during bowel movements, or heavy lifting
Pregnancy and childbirth, which can strain abdominal muscles
Obesity, which increases pressure on abdominal tissues
Age-related muscle weakness
Chronic constipation causing repeated straining
Chronic obstructive pulmonary disease (COPD) causing persistent coughing
Ascites (fluid in the abdomen) creating pressure on the abdominal wall
Genetic factors affecting connective tissue strength (e.g., Ehlers-Danlos syndrome)
Signs & Symptoms
Hiatal hernia: Heartburn, regurgitation, chest pain, difficulty swallowing, and feeling full quickly
Inguinal hernia: Bulge in the groin area that may disappear when lying down, pain or discomfort, especially when bending, coughing, or lifting
Umbilical hernia: Visible bulge near the navel that may be more prominent when coughing or straining
Incisional hernia: Bulge near or at the site of a previous surgical scar, pain or discomfort in the area
General hernia symptoms: Feeling of heaviness, pressure, or weakness in the affected area
Pain or discomfort that worsens with physical activity
Burning or aching sensation at the site of the bulge
Digestive issues including nausea, vomiting, or constipation (particularly with hiatal hernias)
Signs of emergency (strangulation): Severe pain, nausea, vomiting, fever, rapid heart rate, or a hernia bulge that becomes red, purple, or dark
Some hernias may be asymptomatic and discovered during routine examinations