What Causes It?
Defective bladder epithelium - A leaky or damaged protective lining (epithelium) of the bladder may allow toxic substances in urine to irritate the bladder wall.
Autoimmune reaction - The body's immune system may attack the bladder tissue, causing inflammation and pain.
Neurogenic inflammation - Activation of pain-sensing nerves in the bladder can lead to release of substances that promote inflammation.
Mast cell activation - These immune system cells release histamine and other chemicals that can cause bladder inflammation and pain.
Pelvic floor dysfunction - Abnormal function of the pelvic floor muscles can contribute to interstitial cystitis symptoms.
Genetic factors - A family history of interstitial cystitis suggests a genetic predisposition.
Prior bladder trauma - Previous injury to the bladder, such as from surgery or infection, may increase risk.
Spinal cord trauma - Injury to the spine may affect bladder function and contribute to symptoms.
Cross-sensitization with other pelvic organs - Conditions affecting nearby organs like the bowel or reproductive organs may trigger bladder symptoms.
Certain foods and beverages - Some individuals report symptom flares after consuming specific items like coffee, alcohol, citrus fruits, or spicy foods.
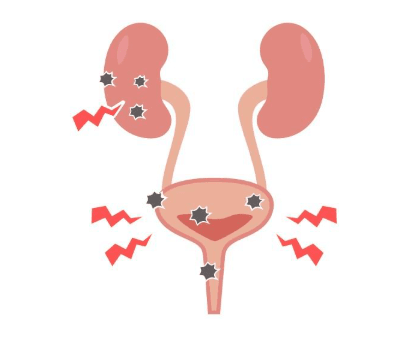
Signs & Symptoms
Chronic pelvic pain - Persistent discomfort in the pelvis, between the navel and thighs.
Bladder pain that worsens as the bladder fills and improves after urination.
Urinary frequency - Needing to urinate more often than normal, sometimes up to 60 times a day in severe cases.
Urinary urgency - A persistent, urgent need to urinate, even immediately after emptying the bladder.
Pain during sexual intercourse - Particularly in women, pain may occur during or after sexual activity.
Dysuria - Painful urination without evidence of infection.
Nocturia - Waking up multiple times at night to urinate.
Small bladder capacity - The bladder may hold less urine than normal.
Symptom flares - Episodes of increased symptoms triggered by menstruation, stress, exercise, sexual activity, or certain foods/beverages.
Pain that changes with bladder filling and emptying - Often worse when the bladder is full and temporarily relieved after urination.
Hunner's lesions - Distinctive areas of inflammation visible on the bladder wall in about 10% of patients.