What Causes It?
Genetic factors - Specific genetic mutations have been identified that can cause Parkinson's disease, though these are relatively rare except in cases with a strong family history of the condition.
Environmental triggers - Exposure to certain toxins or environmental factors may increase the risk of Parkinson's disease, though the exposure generally needs to be significant.
Presence of Lewy bodies - Clumps of specific substances (alpha-synuclein protein) within brain cells are microscopic markers of Parkinson's disease.
Loss of dopamine-producing cells - The death of neurons that produce dopamine, a chemical messenger that helps coordinate movement, is the primary cause of motor symptoms.
Age - Parkinson's disease risk increases with age, with onset typically after age 60, though about 5-10% of cases are early-onset occurring before age 50.
Sex - Men are more likely to develop Parkinson's disease than women, possibly due to hormonal or occupational exposure differences.
Head injuries - Traumatic brain injury may increase the risk of developing Parkinson's disease years after the injury.
Declining estrogen levels - The reduction in estrogen levels in women after menopause may explain the higher rate in men versus women.
Agricultural work - Exposure to pesticides and herbicides in farming has been linked to higher rates of Parkinson's disease.
Industrial chemicals - Exposure to solvents, metals, and other industrial chemicals may increase risk.
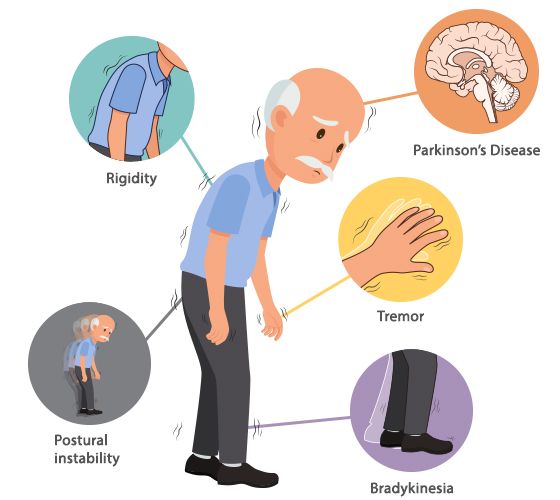
Signs & Symptoms
Tremor - Usually begins in a limb, often the hand or fingers, typically occurring at rest and decreasing with purposeful movement.
Bradykinesia (slowed movement) - Over time, Parkinson's disease may reduce ability to move, making simple tasks difficult and time-consuming.
Rigid muscles - Muscle stiffness can occur in any part of the body, causing pain and limiting range of motion.
Impaired posture and balance - Posture may become stooped, with increased fall risk due to balance problems.
Loss of automatic movements - Decreased ability to perform unconscious movements like blinking, smiling, or swinging arms when walking.
Speech changes - Speaking softly, quickly, slurring, or hesitating before talking; speech may become more monotone.
Writing changes - Handwriting may become small, cramped, and difficult to read (micrographia).
Non-motor symptoms - Including depression, cognitive changes, sleep problems, constipation, and loss of sense of smell.
Facial masking - Reduced facial expression due to affected facial muscles, sometimes called "masked face."
Freezing - Temporary inability to move, especially when initiating movement or encountering doorways or crowded spaces.
Voice changes - Voice becoming softer, more monotone, hoarse, or breathiness while speaking.