What Causes It?
Genetic predisposition - Family history of eczema, asthma, or allergies significantly increases risk, with research in Indian families showing stronger maternal inheritance patterns
Skin barrier dysfunction - Defects in filaggrin and other proteins that maintain skin barrier integrity allow moisture loss and allergen entry
Immune system dysregulation - Overactive immune responses, particularly involving Th2 cells and inflammatory cytokines, trigger skin inflammation
Environmental triggers - Dust mites, pollen, mold, and animal dander often exacerbate symptoms, with house dust mites being particularly problematic in humid Indian climates
Climate factors - Hot, humid conditions common across much of India can worsen sweating and eczema flares; conversely, winter dryness also triggers symptoms in northern regions
Air pollution - Higher rates of eczema in Indian urban centers correlate with increased air pollution, particularly PM2.5 particles
Food allergens - Certain foods may trigger flares in some children, with studies in Indian populations showing egg, milk, and peanut as common culprits
Irritants - Harsh soaps, detergents, synthetic fabrics, and wool can irritate sensitive skin
Stress - Emotional stress exacerbates symptoms through neuroimmunomodulatory pathways
Microbial imbalance - Staphylococcus aureus colonization is more common on eczematous skin and contributes to inflammation and infection
Signs & Symptoms
Intensely itchy skin - The hallmark symptom, often worse at night, disrupting sleep
Dry, scaly patches - May appear red on lighter skin tones or darker brown/purple on darker skin common in Indian children
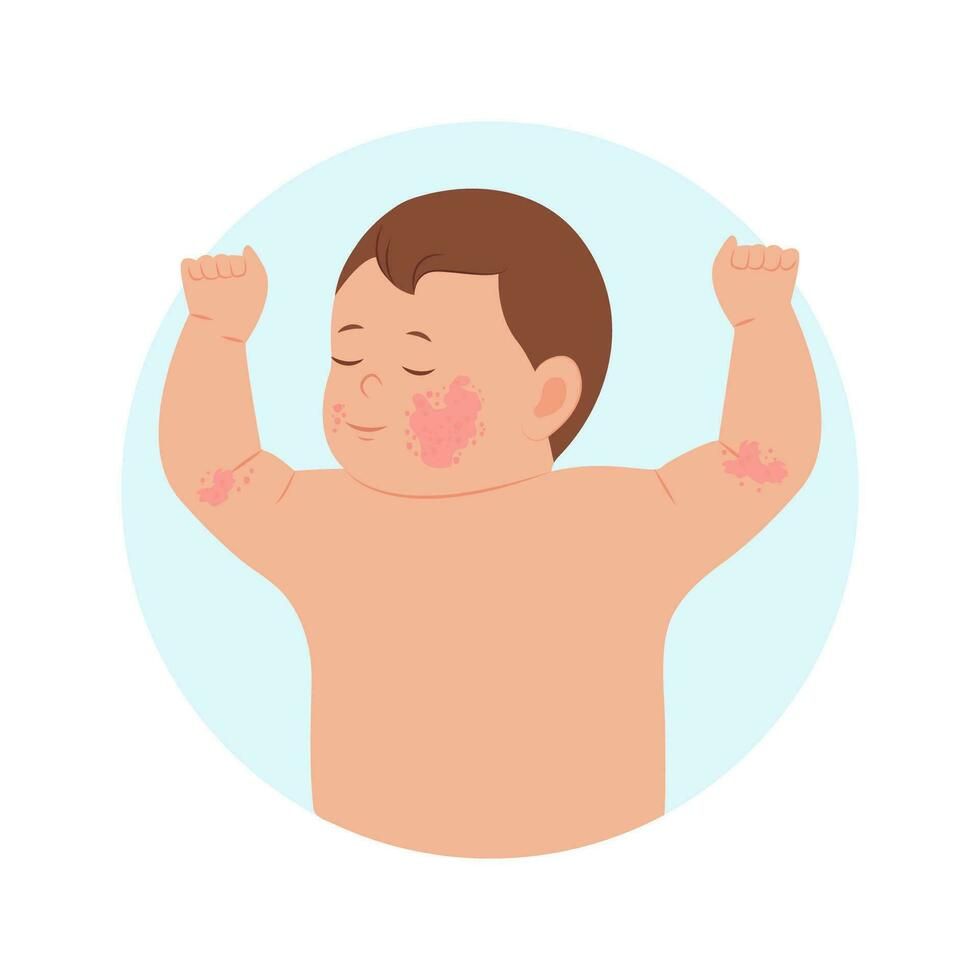
Location-specific rashes - In infants: cheeks, scalp, and extensor surfaces; in older children: flexural areas like neck, wrists, ankles, and behind knees/elbows
Skin thickening (lichenification) - From chronic scratching, more visible as darkened areas in darker skin tones
Post-inflammatory hyperpigmentation - More pronounced in Indian children with darker skin, causing persistent dark patches after inflammation subsides
Frequent skin infections - Due to scratching and compromised skin barrier, with increased risk of bacterial, viral, and fungal infections
Small, fluid-filled bumps - That may ooze and crust, especially during flares
Facial features - Increased infraorbital folds (Dennie-Morgan lines) and darkening around eyes
Hyperlinear palms - Increased palm and sole creases, particularly visible in South Asian children
Xerosis - Extremely dry skin even in non-eczematous areas
Follicular accentuation - Small bumps at hair follicles, more noticeable in darker skin
Heat intolerance - Sweating triggers itching and discomfort, particularly challenging in India's warm climate
Variable presentation - Symptoms may flare and remit, with periods of relative improvement followed by exacerbations